This web page was created as an assignment for an undergraduate course at Davidson College.
Lassa Fever
Figure 1. Lassa virus in vitro. (Woods, 2003)
Introduction
History: Lassa fever, as known as Lassa hemorrhagic Fever,
has been described for decades throughout West Africa, but was first identified
in 1969 upon the illness of two mission nurses in the Jos area of Nigeria. One
nurse died and the second was repatriated to the US and came to a full recovery.
The two nurses worked in the town of Lassa, for which the virus is now named.
The disease is identified in many West African countries (including Guinea,
Sierra Leone, Nigeria, and Liberia), though there have been many outbreaks of
Lassa fever reported since 1969. (McCormick, 1999; Harper, 2002) The disease
is caused by the Lassa virus, an arenavirus of which there are 4 strains: Josiah
(the most studied strain from Sierra Leone), Nigeria, LP and AV. (Durham, 2002)
Much like in Dengue, each strain can cause either a mild reaction in a human
(which occurs in about 80% of the cases) or a severe multi-system infection,
which usually includes hemorrhaging. In the countries with endemic Lassa fever,
it accounts for 10-15% of all hospital admissions. (McCormick, 1999) Though
the mortality rate is normally quite low, it can rise up to 50% at times of
an epidemic. (State Deparment, 2003) The disease is especially deleterious to
women in the third trimester, 95% of which lose the fetus. (McCormick, 1999;
WHO, 2000) The number of infections in West Africa is estimated at 100,000 to
300,000 per year, with about 5,000 deaths, a very rough number, however, due
to the differing recording and diagnosis techniques throughout the regions.
(CDC, 2002)
"The microbe is nothing; the terrain is everything." Louis Pasteur
Figure 2. Map of the areas in West Africa endemic for Lassa fever. (McCormick, 1999)
Transmission: The Lassa virus is transmitted to humans through the animal host known as the “multimammate rat” of the genus Mastomys, of which there are at least 2 vector species; M. huberti and M. erythroleucus. (State Deparment, 2003) These rodents reproduce at very high rates and like to live in very close proximity to humans, especially where food is kept. They shed the virus in their urine and droppings. Contact with the virus may occur through infected food, the inhalation of viral particles in the air, and even through consumption of Mastomys rats as a food source. Person-to-person infection may occur when someone comes in contact with the blood, tissue, secretions, or excretions of an infected individual. (CDC, 2002) The incubation time of the virus in humans can range from 6-21 days, and due to this prolonged period, this is one of the most “imported” viruses in the world. Travelers do not fall sick until weeks after exposure to the virus, and this has led to the spread of the virus both to the US, to Chicago in 1989, and Germany as the most well documented cases of its spread. (McCormick, 1999) The virus has been isolated from human blood up to 19 days after infection and from urine up to 32 days after infection. (Fabiyi, 2003) The virus can be excreted in the urine of patients for three to nine weeks after the onset of the disease and can be spread through semen for up to three months. (WHO, 2000)

Figure 3. Mastomys rodent, also known as the "multimammate" rat. (CDC, 2002)
Symptoms: The clinical presentation of Lassa fever is very
non-specific. Symptoms include: fever, malaise, headache, sore throat, nausea,
vomiting, diarrhea, myalgia, proteinuria, and chest and abdominal pain. Severe
cases result in hypotension, pleural effusion, hemorrhage, seizures, encephalopathy,
and swelling of the face and neck. (CDC, 2002; WHO, 2000) Complications of the
disease after recovery include hair loss, loss of coordination, psychiatric
syndromes (such as mania, depression, dementia, psychosis and sleep disorders)
and the most common, deafness, which occurs in 1/3 of the patients. Lassa Fever
is therefore a hemorrhagic, hepatic, and neural disease. (Solbrig, 1993)
Diagnosis: Because the symptoms of Lassa Fever are non-descript
and hard to differentiate between those of malaria, yellow fever, and other
hemorrhagic fevers, definitive diagnosis requires laboratory work. (WHO, 2000)
ELISA tests and reverse transcriptase PCR are used when available for decisive
diagnosis. An AST test is also very useful since Lassa patients exhibit raised
liver enzymes in their urine. (McCormick, 1999)
Arenaviruses
The Lassa virus is classified as an arenavirus. Arenaviruses are enveloped,
bisegmented RNA viruses with a granular appearance. They are all pathogens of
rodents, in which they cause no disease symptoms. (Woods, 2003) There are 11
classified members of the arenavirus family, all divided into 2 groups rather
arbritrarily: Old World and New World. Lassa is an Old world virus, though the
distinction is rather capricious since there is exists a lot of crossreactivity
of the viruses due to the common epitopes found on their nucleocapsid protein.
Lassa is most closely related to LCMV (lymphocytic choriomeningitis virus),
shown through the complement fixation test. Because of this, LCMV is commonly
used as a model in the studies of Lassa fever. (Oldstone, 2002; Howard, 1993)
Lassa is a negative RNA virus, meaning that its genome does not participate
directly in protein synthesis. (Garcin, 1993)
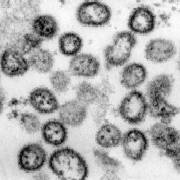
Figure 4. Lassa Virus. (WHO, 2000)
Immunological Aspects (Pathology)
The Lassa virus enters the human
body through multiple venues, including the bloodstream, lymph vessels, repiratory
tract, or the digestive tract. There are many curious aspects of the pathogenesis
of Lassa, though it is still not fully understood. Neutrophil and total leukocyte
counts are usually low in the primary infection, but rise with growing tissue
damage. (Woods, 2003) The immune response to Lassa is a cell-mediated one, though
specific antibodies, mainly IgM, can be found. These appear only weeks after
primary infection and don’t play a role in the primary acute response.
Specific antibodies are persistent for four to five years after infection. (Fabiyi,
2003) Lassa specific antibodies simply neutralize the antigen and target it
for removal. The Lassa virus readily infects vascular endothelial cells and
macrophages. Viral peptides are presented through MHC class I molecules and
therefore CD8 T cells play the critical role in the suppression of the primary
infection. (Oldstone, 2002) Viral replication in the reticuloendothelial cells
causes capillary lesions, which lead to erythrocyte and platelet loss, increased
vascular permeability and hemorrhage in various organs. (Harper, 2002) In platelet
function tests of Lassa patients, the infected platelets do not aggregate, thus
clotting throughout the body is impaired and the body is exposed to hemorrhaging.
(McCormick, 1999) The degranulation of both platelets and neutrophils is inhibited
upon infection. (Solbrig, 1993)
In a recent investigation Mahanty, et al., studied whether pro-inflammatory cytokines and chemokines secreted by macrophages, endothelial cells, and other immune cells were present in Lassa fever patients, and then correlated their presence with disease severity. In this study it was shown that patients with nonfatal Lassa fever showed elevated levels of IL-8 and the IFN-inducible protein IP-10 until the resolution of the disease, whereas patients with fatal Lassa fever had almost undetectable levels of these chemokines throughout the course of their illness. This data suggests that patients with fatal Lassa have a weak pro- and anti- inflammatory response, especially once they are hospitalized. This data correlates with the fact that macrophages are one of the classes of cells first infected, and it has been shown that they produce IL-8 as early as 24 hours after infection. The infection of macrophges by Lassa virus causes a decrease in the secretion of IL-8. IL-8 is a CXC chemokine also secreted by monocytes, neutrophils, and endothelial cells, which functions as a chemo-attractant for neutrophils and T-cells. IL-8 is thought to be very important in neutrophil degranulation and T cell activation. As stated above, neutrophil levels are very low in fatal Lassa patients. IP-10 is also a CXC chemokine secreted by macrophages, endothelial cells, and T cells in response to other cytokines. It is believed to play a role in the pathogenesis of infections and shock through the inhibition of endothelial cells function and the chemo-attraction of T cells and NK cells. “These mediators therefore are likely to account for many of the nonspecific features of Lassa fever that make it so difficult to differentiate the disease from other infections in its early phases.” (Mahanty, et al., 2001)
Figure 5. Chime image of IL-8, inflammatory mediator with suspected role in the pathogenesis of Lassa Fever. (Clore, et al.)
The Lassa virus also attacks the central nervous system and opens the body up to infection by other pathogens, such as malaria. (Garret, 1994) The neurological and psychiatric effects of the virus result from its attack of the CNS. This can result from several limitations of the blood-brain barrier, including documented cases of the virus crossing into the cerebrospinal fluid through the blood if subarachnoid hemorrhage occurs. There are also areas in which the blood-brain barrier is lacking, including the pituitary, pineal, area postrema, supraoptic crest, and subfornical organ, sites which match the neuropathological effects of Lass fever, though this has not yet been proven. (Solbrig, 1993)
Treatment
"When the tide is receding from the beach it is easy to have the illusion that one can empty the ocean by removing water with a pail." Rene Dubos
Plasma Therapy: Plasma therapy was the first attempted treatment
for Lassa fever. This treatment involves taking the blood of recovered Lassa
victims, separating out the plasma, including antibodies, and injecting it into
the current victim. This process has been used with varying degrees of success
in both Lassa patients and those of other arenaviruses, including Junin, the
culprit in Argentine Hemorrhagic Fever. (McCormick, 1999; Garret, 1994)
Ribavirin: In 1979, Dr. Joe McCormick pushed through the approval
of testing of a drug called ribavirin, until then only tested in primates, for
use in the field in the heart of Lassa country, Sierra Leone. Ribavirin is a
drug that interferes with viral replication and viral protein synthesis. It
has been by far the most effective treatment for patients with severe Lassa
fever through both oral and intravenous means. (McCormick, 1999) Ribavirin reduces
viraemia, though does not eliminate it, and is most effective early on in the
infection. (Woods, 2003) Prostacyclin is another drug still under investigation
that protects platelet function. (McCormick, 1999)
Vaccines: “Early diagnosis of Lassa Fever is difficult
and effective treatment is not available, thus vaccination is a rational strategy
to control the disease.” (Buchmeier, 2000) The Lassa virus induces a cell-mediated
immune response. There have been multiple investigations into the production
of a vaccine, seeing as it would be the best preventative measure to fight this
disease. Irradiated virus vaccines have no effect in protecting animals from
Lassa. Live attenuated vaccines are a possibility, but they are unavailable,
so most of the research has turned to recombinant virus vaccines. (Auperin,
1993) Bivalent vaccines using modified alphavirus replicons have been proven
to protect animals against both Lassa and Ebola infection. (Greer, 2002) Extensive
research has been made into DNA vaccines. Using competitive binding assays,
researchers have been able to identify multiple peptides and determine their
affinity for HLA alleles. A total of 34 MHC-I binding peptides have been identified.
The injection of DNA vaccine constructs using these peptides resulted in immune
responses, both humoral and T-cell, in mice. (Buchmeier, 2000)