This web page was produced as an assignment for an undergraduate course at Davidson College.
Pharmacogenomics is an intersection of the fields of pharmacology and genomics that deals with predicting how individual patients react to administered medicine, with the end goal of optimizing drug dosage and administration intervals for maximum healing efficacy and minimum harm to the patient. In most simple terms, just like a child is different from an adult in that it cannot (and must not be required to) tolerate drugs of the same dosage based on its body mass, so is any person different from the next one based on their genetic makeup. In order to make personalized predictions possible, pharmacogenomics therefore studies the patient’s genome in relevance to the drug’s mechanistic properties, such as metabolism, method of impact and side toxicity.
Enzymes such as members of the cytochrome p450 family have been known to have a pronounced impact on the metabolism of various drugs. By studying the cytochrome p450 genes and their expression patterns in a patient, pharmacogenomicists are able to characterize him as an “extensive”, “intermediate, ultra-rapid, and poor” metabolizer, and hence personalize his treatment to an appropriate dosage and interval of administration of the drug. (Hart et al., 2008)
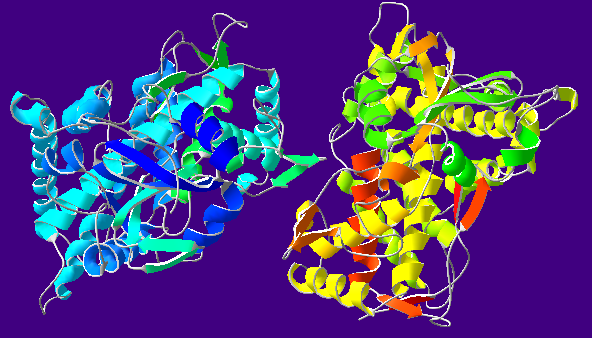
Cytochrome P450 Oxidase (CYP2C9).
Image courtesy of Wikimedia Commons.
It is always possible that a drug might not have the desired effect on a patient due to a mechanical impossibility. If, for example, the patient has a mutated gene encoding for the receptor that the drug is targeted to, the drug might not be able to bind to it properly, if at all. Nevertheless, determining whether a medicine will be effective or not has this far not been prioritized by the field. Such analysis might come at a cost to the patient, as it requires time that might be better spent on the patient's treatment instead. Therefore, to prevent such inefficiency, the default option has been to simply administer the recommended drug first and see what happens. While this approach does not require time for sophisticated analysis, it also carries an inherent risk to the health of the patient. In case the drug is counterindicative to some unkown condition that the patient might have which is not immediately obvious, the aftermath of its administration could be irreversible. It is estimated that, in the US only, more than 100,000 patient deaths are attributable to such adverse drug reactions.(Lazarou et al., 1998) Increasing the contents, functionality, and accessibility of pharmacogenomical methods and databases has the potential to prevent many of these fatalities and tilt the prescription cost-benefit analysis in favor of making a sound judgment on a drug’s effectiveness before administering it.
There is increasing evidence that the polymorphic character of genes involved in the metabolism of certain drugs, such as CYP2D6 (which metabolizes Tamoxifen, a common medication prescribed to breast cancer patients), is correlated with health risks arising from toxicities upon drug intake. (Lee et al., 2011) Such adverse effects can be easily prevented through genomic screening of the relevant loci.
Clinical trials aimed at characterizing drug efficiency and potential harms have historically been conducted in patients predominantly identifying themselves as White Caucasians. (Bradford, 2008) Variations in drug response have been documented to correspond to patients' racial or ethnical belonging on the basis of both physiological and cultural differences. (Food and Drug Administration, 2005) Unaccounted for variations have resulted in an unequal quality of healthcare that better catters to the needs of the majorities. Nevertheless, it is the minorities that are more needy. In order to prevent such unequity, the Food and Drug Administration has recommended that clinical trials of all stages be conducted in comprehensive groups inclusive of the most common underrepresented groups in the population that the drug being tested is targeted to. (Food and Drug Administration, 2005) No legislation has yet been passed to mandate such regulations, however.
Much like any other rapidly progressing field, pharmacogenomics (and the field’s increasing demand for genotyping) has not been able to avoid criticism over its possible future implications.
On the ethical side, the possibility remains that genetic typing might pave the way to a novel form of stereotyping, such as the one predicted by the popular science-fiction movie Gattaca. There is already evidence that insurance agencies are using genetic screening data to influence the costs of life and health insurance for their clients. (Keough et al., 2013) Fortunately, with the establishment of the Council for Responsible Genetics (CRG) and the passage of The Genetic Information Nondiscrimination Act of 2008, such instances have been largely limited, yet the risk remains.
On the practical side, the issue concerning pharmacogenomics is not any less complicated. In the light of the rapid progress of the field, it is of utter importance to keep in mind that change is one of the key properties of life as we know it. People, just like all other organisms known to evolution, exist in a dynamic that constitutes their characteristics as only transitory. Therefore, in the quest for obtaining more and more information regarding a single patient’s genes and expression patterns, we must ask: Where do we stop?
Bradford, L. DiAnne. "Race, Genetics, Metabolism: Drug Therapy and Clinical Trials." MIWatch.org. MIWatch, (2008) n.d.
"Genes/Stereotypes." Rev. of Gattaca. Web log post. Gattaca Reflections. N.p., n.d.
"Genetic Discrimination." CRG. ©2001, Council for Responsible Genetics., n.d.
Hart, S. N., S. Wang, K. Nakamoto, C. Wesselman, Y. Li, and X. B. Zhong. ""Genetic Polymorphisms in Cytochrome P450 Oxidoreductase Influence Microsomal P450-catalyzed Drug Metabolism"" Pharmacogenetics and Genomics 18.1 (2008): 11-24.
Keogh, Louise A., and Margaret F A Otlowski. "Life Insurance and Genetic Test Results: A Mutation Carrier's Fight to Achieve Full Cover." Medical Journal of Australia 199.5 (2013): 363-66.
Lazarou, Jason, Bruce H. Pomeranz, and Paul N. Corey. "Incidence of Adverse Drug Reactions in Hospitalized Patients." The Journal of the American Medical Association 279.15 (1998): 1200-205.
Lee, Soo-Youn, and Howard L. McLeod. "Pharmacogenetic Tests in Cancer Chemotherapy: What Physicians Should Know for Clinical Application." The Journal of Pathology 223.1 (2011): 15-27.
USA. Equal Employment Opportunity Commission. The Genetic Information Nondiscrimination Act of 2008. Senate and House of Representatives, n.d.
USA. Food and Drug Administration. Collection of Race and Ethnicity Data in Clinical Trials. N.p.: n.p., 2005.
Genomics Page
Biology Home Page
© Copyright 2014 Department of Biology, Davidson College, Davidson, NC 28035