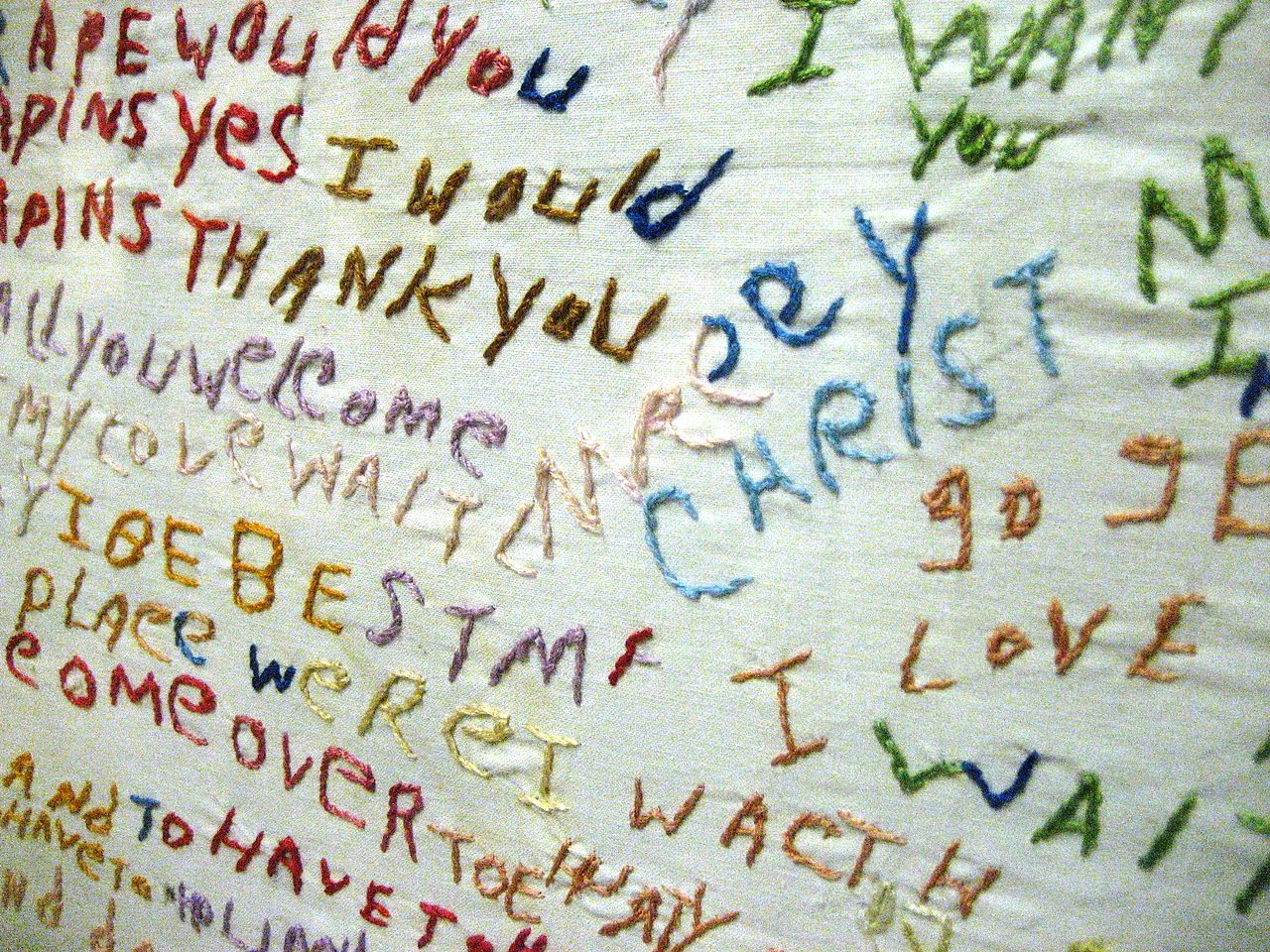
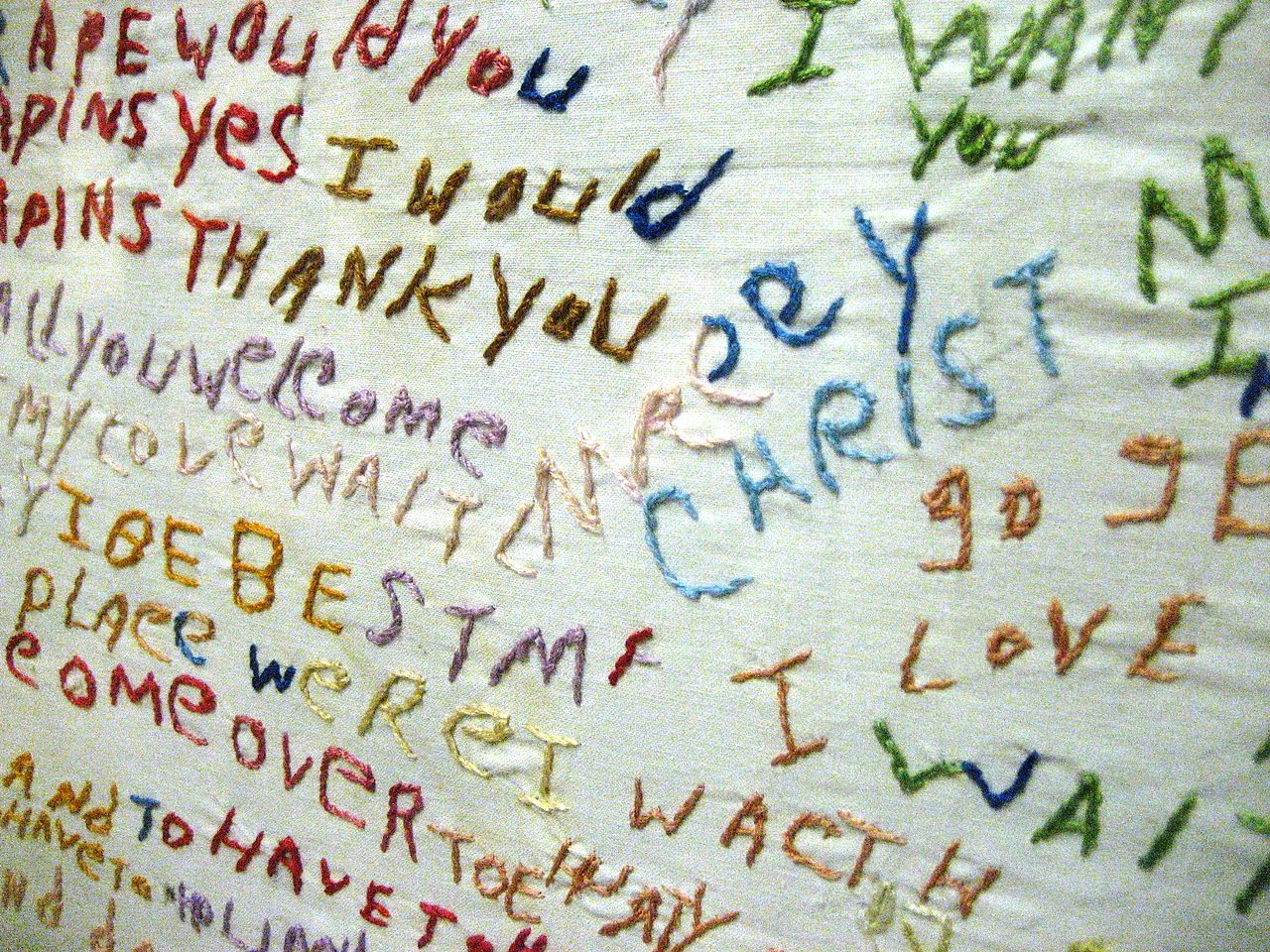
Figure 1. Embroidery by a person diagnosed with schizophrenia.
Those diagnosed with schizophrenia typically suffer from delusions, hallucinations,
and/or disorganized speech. Image courtesy of Wikimedia Commons.
This web page was produced as an assignment for an undergraduate course at Davidson College.
Back to the Past in Schizophrenia Genomics
Genomic-epigenomic
Interactions Driving Risk for Schizophrenia
Schizophrenia is a neuropsychiatric disorder that is
clinically well characterized but has a poorly understood
neuropathology. It is believed to be in part of genetic origin, and
increased risk for schizophrenia may be acquired during early
development, despite the fact that the disease does not typically
manifest until adulthood (Jablensky, 2010). In January of 2016, two
separate genomics research projects conducted in two separate labs were
evaluated, and their results were taken together to draw new conclusions
about the potential epigenomic influence on the etiology of
schizophrenia. The two studies employed slightly different techniques to
investigate the effect the changes in DNA methylation occurring in the
prenatal to postnatal transition during development may have on brain
development of those with and without schizophrenia. Furthermore, the
studies sought to assess the influence of variations in DNA sequence on
DNA methylation via identification of methylation quantitative trait
loci (meQTLs), genomic loci where genotypic variation may affect
patterns of DNA methylation (Smith et al., 2014).
Simultaneous
Hypothesis Driven and Discovery Science
In both studies, the researchers were testing a
hypothesis. The most heavily supported hypothesis to describe the
pathology of schizophrenia, the neurodevelopmental
hypothesis, postulates that risk for schizophrenia is at least in
part a result of abnormalities in early brain development (Fatemi &
Folsom, 2009). Additionally epigenetic dysregulation of gene expression
have been associated with a variety of neurodevelopmental disorders,
including schizophrenia. Both studies examined the relationship between
the epigenomic regulation, specifically DNA methylation, and genetic
risk for schizophrenia. This information led the researchers in both
studies to test the hypothesis that DNA methylation changes in
prefrontal cortex will occur in development as early as the prenatal to
postnatal transition.
However, the researchers in both studies were also
doing discovery science at least to an extent, as they each sought to
identify loci where genotype may be influencing DNA methylation, and
perhaps the subsequent level of risk for schizophrenia. In these
experiments specifically, the researchers were only driven by the
hypothesis that genotype may influence DNA methylation. The exploration
of where in the genome this may occur and to what extent was purely
discovery science in both studies.
Genomic Technology Employed In These Studies
In both projects, the same genomic technologies were employed. The two projects then differed how the researchers analyzed the data obtained using these technologies and in the specific trends they were looking for. In both studies, a methylation microarray was used to assess DNA methylation in the prefrontal cortex tissue samples. The methylation microarray is a chip similar to the well-known DNA microarray chip, but it specifically measures genome-wide CpG methylation. The researchers also employed SNP arrays to assess genotypes, and subsequently haplotypes, of DNA obtained from cerebellar tissue samples. The data obtained from these two genomic arrays were taken together to analyze the effect of genotype on levels of DNA methylation via eQTL analysis.Take
Home Message
Genomic technology has allowed us to examine the
interaction between epigenomic regulation in the form of DNA methylation
and predisposition to a neuropsychiatric disease. DNA methylation, or
lack thereof, can change rates of gene expression, thus altering the
development of the tissue in which the genes are expressed. When
dysregulation occurs during a critical developmental time point in a
particular tissue, the development of that tissue may be altered or
hindered in some way. When this epigenomic dysregulation occurs in the
brain, it is not surprising that risk for a neuropsychiatric condition
such as schizophrenia may be the result. It is important to note that
DNA methylation is not the only form of epigenomic regulation, but it is
the one that has been most heavily implicated in the neuropathology of
schizophrenia to date. Furthermore, there are specific genomic sequences
that influence the epigenome. Those that influence DNA methylation
levels are meQTLs. Thus, one of the biggest overall takeaways from these
two studies is that they highlight both the interconnectedness of the
genome and epigenome and the complexity of the interactions between
them.
Evaluation of Projects
I think the projects discussed in this article are valuable on two
levels. First, they utilize genomic technology to uncover new and
valuable information about the genetic component of the etiology of
schizophrenia. Ultimately, the findings can help us narrow down the
developmental time window in which humans become most susceptible to
increasing their risk of later developing schizophrenia and potentially
identify genomic locations that serve as markers for genetic risk for
the development of schizophrenia in adulthood. Neither of the projects
absolutely determined the manner in which the genome, epigenome, and
interactions between the two may influence risk of schizophrenia, nor
did they claim to. However, both projects provide evidence that there is
likely a genomic-epigenomic component to the etiology of the disease.
Although there is much more work to be done, the steps taken in these
two projects are important ones for initiating additional research into
the genomic-epigenomic interactions that may impact an individual's risk
for developing schizophrenia.
Second, these studies demonstrate the immense value
genomics brings to furthering our understanding of complex biological
processes. These two projects sought to examine the potential effect of
genomic variations on epigenomic regulation and in turn on variations in
gene expression during early brain development that may later contribute
to the development of schizophrenia. In doing so, they made a valuable
impact on our understanding of the biological basis of a disease that
has been clinically characterized for over a generation, but never fully
understood from a neuroscientific standpoint (Jablensky, 2010). Thus,
the studies highlight the widespread potential of genomic research to
shed light on the biological mechanisms and genetic bases of diseases,
functions, and processes that have to date remained scientific
mysteries.
References
Fatemi SH, Folsom TD. 2009. The neurodevelopmental hypothesis of
schizophrenia, revisited. Schizophr Bull. 35(3):528-548
Jablensky A. 2010. The diagnostic concept of schizophrenia: its history,
evolution, and future prospects.
Smith AK, Kilaru V, Kocak M, Almli LM, Mercer KB, Ressler KJ, Tylavsky
FA, Conneely KN. 2014. Methylation quantative trait loci (meQTLs) are
consistently detected across ancestry, developmental stage, and tissue
type.
Abstracts
Methylation
QTLs & Schizophrenia Risk
Genomics
Page
Biology Home Page
Email Questions or Comments: moshannon@davidson.edu
© Copyright 2016 Department of Biology, Davidson College, Davidson, NC 28035