|
|
Ever since ancient times, leprosy has been one of the most hated diseases. Leprosy, also known as Hansen disease, is a chronic infectious disease that, if left untreated, can cause debilitating deformities and slowly progress throughout one's life. Leprosy is characterized by peripheral nerve damage and cutaneous lesions. In order to contract the disease, one has to live in close contact with an infected individual for a prolonged amount of time (Mooney, 1999). These physical effects paired with the social stigma of being infected with this dreaded disease, often lead to those affected being afraid to come forward to seek treatment in the early stages of the disease.
How is Leprosy Transmitted?
The bacillus Mycobacterium leprae causes leprosy. Mycobacterium leprae was discovered in 1873 by G.A. Hansen
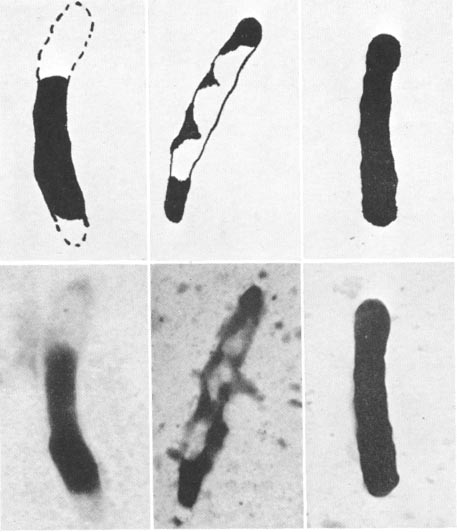 |
(hence the disease was subsequently named after him). At that time, it was the only bacterium that had been discovered to cause a human disease (Leprosy: the Disease, 2000). Rod-shaped with rounded ends, Mycobacterium leprae occurs in large numbers, often grouped in bundles, in the lesions of patients with lepromatous leprosy. The bacilli also group in clumps surrounded by a capsule called globi, located both in intracellular and extra-cellular spaces. Viable bacilli stain with carbol-fuchsin as solid rods, whereas bacilli that stain irregularly are probably dead (Microbiology of Mycobacterium leprae, 2000). In the photograph to the left the top images are drawings of the human leprosy bacilli seen under a microscope in the bottom row. The right images show that the bacillus is viable because it is uniformly stained. Both the left images with beaded staining and the middle images with empty cell walls at the extremities are dead forms of the bacillus. The Mycobacterium leprae grows in the vessicles within macrophages which must be activated by TH1 cells (Janeway, 1999). Photograph courtesy of Wolstenholme et al |
The bacteriological index (BI), calulated by counting six to eight stained smears, shows how much bacillus is present. The smears are made by cutting the skin around the infected area with a scapel and scraping fluid and tissue from it. This sample is them evenly spread on a slide and stained by the Ziehl-Neelsen method. The bacilli are then counted and expressed in a logrithmic scale. The BI is useful because the results are representative of many of the infected individual's lesions (Microbiology of Mycobacterium leprae, 2000).
The only known reservoir of this bacillus is humans, but diseases caused by bacilli indistinguishable from M. leprae have been discovered in armadillos of the southern U.S. (Transmission of Leprosy, 2000). It is not know, however, it these bacili can cause leprosy in humans. Although the direct means of transmission between humans is unknown, it is believed that the bacillus is expelled from the nose in respiratory droplets or from sores and thus can be spread through direct skin contact or by inhalation (Encyclopaedia Britannica, 2000). Individuals with lepromatous leprosy have an enormous amount of bacilli, reaching to over seven billion organisms per gram of tissue (Transmission of Leprosy, 2000). Mycobacterium leprae from nasal secretions can live outside of the human host for thirty-six hours, or as much as nine days in tropical climates. It is quite difficult, however, to determine when the bacillus was contracted because it has an incubation period of about five years, but it may take as many as twenty years for symptoms to develop (www.who.int/inf-fs/ed/fact101.html, 2000). It has been found that leprosy is not a highly contagious disease. In fact, many adults that live in leprosy-affected areas seem to be immune, but children are more susceptible (www2.adam.com/ency/article/001347.htm, 2000).
Two Subdivisions of Leprosy
Leprosy can be subdivided into two forms, lepromatous leprosy and tuberculoid leprosy, the less destructive of the two. In tuberculoid (or paucibacillary) leprosy, body cells try to prevent the spread of bacillus by crowding into the area of infection. In these patients, TH1 cells are induced to respond, thus activating the macrophages to destroy
 |
the bacillus (Janeway, 1999). Very few bacilli can be detected in these areas. (Photograph courtesy of LEPRA) As a result, very large nodules called tubercles are formed under the skin's surface. The tubercles look like a dense dry spot which cannot sense hot, cold, or touch because the skin's nerve fibrils are involved as well. As the disease slowly progresses, inflammation surrounds the main trunk of the nerve so that nerve impulses cannot travel up or down. The infected individual looses pain sensation, blood circulation, and muscle power in the infected area (Encyclopaedia Britannica, 2000). The |
| fingers become stuck in a clenched position which may be straighted either with plaster casts or, in the more severe cases, tendon transfer surgeries (Mooney, 1999). If the affected nerve is in the lower leg, drop feet are common (Photograph courtesy of Mooney). When this occurs, the individual is unable to lift his or her foot whenwalking. Because the patient cannot sense pain, minor cuts go uncared for and turn into larger problems. (Photograph courtesy of LEPRA). As a result, the toes can be severly damaged by large, eroding ulcers. Many times the toes either deteriorate on their own or are amputated (Mooney, 1999). This entire process is caused by the immune response which, although it prevents the bacilli from spreading, causes immense tissue damage in the infected areas. Interestingly, |  |
|
|
|
Department
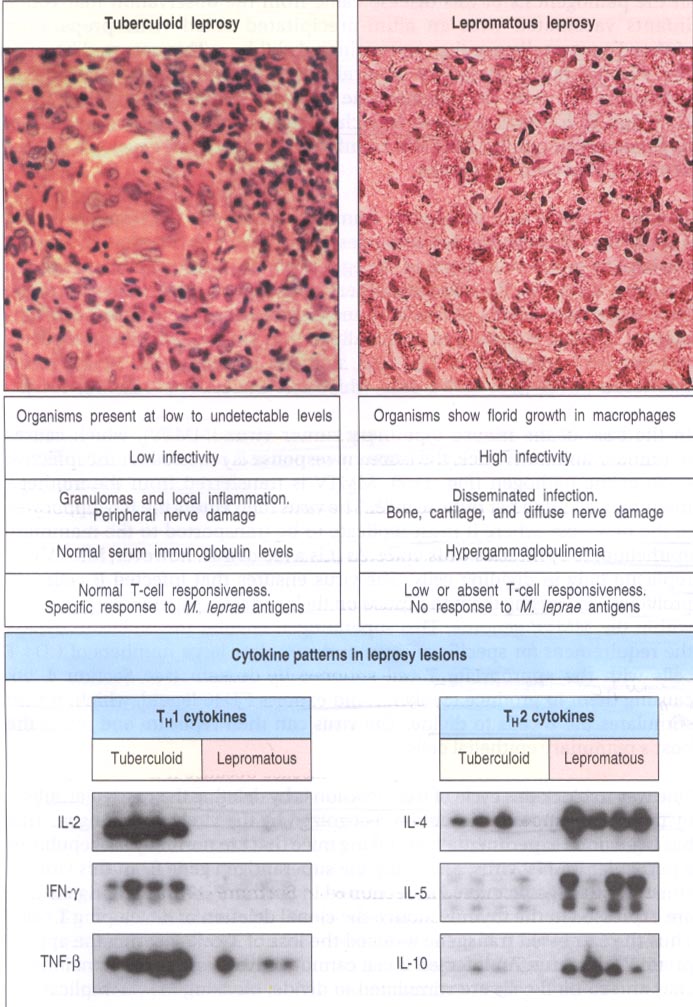
of Health and Human Services, 1980). This figure shows the macrophage
and T-cell responses to Mycobacterium
leprae during the two types of leprosy infections. On the left
is turberculoid leprosy, the less severe of the two. TH1
cells are preferentially activated to control the infected areas.
These cells release IL-2, INF-gamma, and TNF-beta. Granulomas are
located inside the lesion. Patients with tuberculoid leprosy experience
local imflamation. On the right is lepromatous leprosy. TH2
cells are activated so the bacilli grow unchecked inside the macrophages.
The infection therefore spreads throughout the body causing bone, cartilage,
anf nerve damage. The TH2 cells release IL-4, IL-5, and
IL-10.
Permission requested from Janeway
et al
|
 |
Leprosy Around the World
Leprosy is often found in conditions connected
with poverty: overcrowding, poor sanitation, and insufficient nutrition
(<www.anandgram.org>). According to
current WHO data, the current global prevalence rate is around 1.4 cases
per 10,000 people. Around 500,000 new cases of leprosy are registered
each year, about 300 of which are in the United States. WHO has mounted
a compaign to try to eliminate Hansen's disease . Elimination is
defined as less than one case per 10,000 people (Ahmad,
1999). Of the twenty-four countries where leprosy is endemic,
twelve will meet the elimination goal by the end of the year 2000.
These countries are Cameroon, Chad, Congo, Cote d'Ivoire, Ethiopia, Gabon,
Gambia, Guinea Bissau, Mali, Papua New Guinea, Paraguay, and Sierra Leone.
The remaining twelve are Angola, Brazil, Central African Republic, Democratic
Republic of the Congo, India, Indonesia, Guinea, Madagascar, Mozambique,
Myanmar, Nepal, and Niger. These coutries account for 90% of the
global prevalence (www.who.int/inf-fs/en/
fact101.html, 2000).
India alone has about 500,000 infected people, which represents 63% of
the global occurances and 87% of the cases for that region (Kumar,
1999).
Map showing where in the World leprosy is most prevalent
Treatment of Leprosy
In the 1940s, scientists discovered that the
drug dapsone stopped the progress of leprosy. Dapsone is an antibiotic
inhibites "folic acid synthesis by inhibition of dihydropteroate synthetase"
(www.hopkins-aids.edu/
publications/book/ch6_dapsone.html,
2000). Treatment with this drug required that the patient take
dapsone for many years. Drug-resistant
Mycobacterium leprae
was found in the 1960s, thus the only treatment available became useless
in some cases. Luckily, soon afterwards, rifampicin and clofazimine
were found to very effective. Rifampin, an antitubular drug stops
the progression of leprosy so that the individual is no longer contagious
and clofazimine reduces the number of mycobacteria in circulation (www.aidsinfonyc.org/network/access/drugs/clof.html).
| (photograph courtesy of LEPRA) Some instances have been recorded where the bacilli has become drug resistant, but these times are typically when the drug treatment schedule is not followed correctly (Encyclopaedia Britannica, 2000). In 1982, the World Health Organization (WHO) began recommending multidrug therapy (MDT) for leprosy patients. MDT contains three drugs, clofazimine, dapsone, and rifampicin which kill "the germ, cures the patient and prevents the occurrence of drug resistance" (www.who.int/inf-fs/en/fact101.html, 2000). !f MDT is started as soon as symptoms are detected, deformities can be avoided. MDT is very effective for another reason; it makes the individual non-infectious after the first treatment. Individuals with tuberculoid leprosy can be cured during a six month course of MDT while patients with lepromatous leprosy require twelve months (www.who.int/inf-fs/en/fact101.html, 2000). In July of 1998 the U.S. Food and Drug Administration approved the use of thalidomide for leprosy treatment as an |
Possibilities for the Future
In order for leprosy to be fully eliminated, many steps need to be taken to integrate the treatment of leprosy into the services for general health. In addition, the stigma attached to be infected needs to be purged from all societies so that infected individuals will seek help rather than spreading the disease to more people. Because cytokines regulate the delicate balance between TH! and TH2 cells, it could be possible to induce the less severe form of leprosy by giving the right cytokines. In a patient with lepromatous leprosy, a cell-mediated response can be induced by administering T-cell growth factor IL-2 or IFN-gamma which induces macrophage activation. Another way would be to give !L-12 which is normally produced by macrophages to induce TH! cells. The idea of injecting cytokines into lesions
|
shows promise
because it has been shown to reverse the type of leprosy (Janeway,
1999). Moveover, a significant amount of research must be done because
the methods of transmission continue to be unknown and also no one has
been able to grow the bacillus in the laboratory. It is possible
to grow the leprosy bacillus in the footpads of mice. This allows
researchers to study the effects of drugs on the disease (Wolstenholme
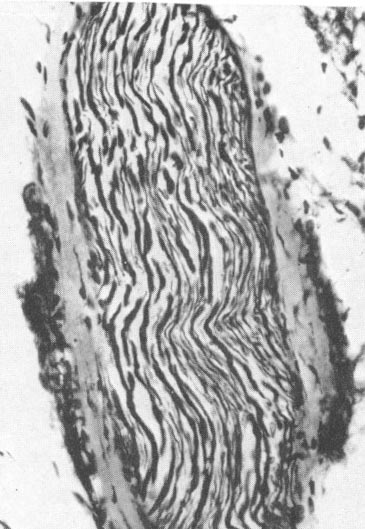
et al, 1963). This photgraph is a section of nerves in the infected
and deformed rear limb of a mouse that has been injected with the bacilli.
The section indicates nerve degeneration, showing proliferation of endoneural
nuclei and fragmented fibers.
Courtesy of Wolstenholme et al |
 |
Links to Related Sites
- Link to Lepromin
skin test
- Center for Disease
Control (CDC) in Atlanta, Georgia.
- World Health
Organization (WHO)
- Anand
Gram: Village of Joy
- British
Leprosy Relief Mission (LEPRA)
- Link to haikus
about leprosy
- Summary of 7th WHO Expert
Committee on Leprosy
- "About Leprosy." <www.anandgram.org>
Accessed on April 17, 2000.
- Ahmad, Khabir 1999. "WHO initiates global
leprosy health-care alliance." Lancet 354: 1802.
- "Clofazimine." <www.aidsinfonyc.org/network/access/drugs/clof.html>
Accessed on April 20, 2000.
- "Dapsone." <www.hopkins-aids.edu/publications/book/ch6_dapsone.html>
Accessed on April 20, 2000.
- Janeway, CA, P Travers, M Walport, JD Capra.
Immunobiology: The Immune System in Health and Disease. New York:
Garland Publishers, 1999.
- Kumar, Sanjay 1999. India falls short
of World Health Organization leprosy targets. Lancet 353: 652.
- LEPRA (British Leprosy Relief Mission). <www.lepra.org.uk/home.html>
Accessed on April 16, 2000.
- "Leprosy." Morbidity and Mortality Weekly
Report 48: 174 (1999).
- "Leprosy." <www2.adam.com/ency/article/001347.htm>
Accessed on April 16, 2000.
- "Leprosy." <www.who.int/inf-fs/en/fact101.html>
Accessed on April 17, 2000.
- "Leprosy: the Disease." <www.who.int/lep/disease/disease.htm>
Accessed on April 17, 2000.
- "Leprosy (Hansen's disease)." Encyclopaedia
Britannica. New York: Encyclopaedia Britannica, 1998.
- "Leprosy (Hansen's disease)." Bethesda,
MD: U.S. Department of Health and Human Services, 1980.
- "Microbiology of Mycobacterium leprae" and
"Transmission of Leprosy." <www.who.int/lep/disease/
Microbiology.micro.htm>
Accessed on April 16, 2000.
- Mooney, Virginia N. (1999). The photographs
and information were collected during a summer spent at the All Africa
Leprosy & Rehabilitation Training Center (ALERT). I performed
operations on patients with leprosy (mainly amputations and tendon transfers)
and worked in physical therapy to monitor the progress of the disease and
to put plaster casts on the patients with claw hands.
- Wolstenholme, G.E. and M. O'Connor.
Pathogenesis of Leprosy. Boston: Little, Brown and Company, 1963.
- Wright, Karen 2000. "Thalidomide is back."
Discover 21: 31-33.
Questions, comments - contact: gimooney@davidson.edu